Part I: One small step for mankind, one giant leap for an analyst
What is a clinical trial and who are involved?
As most of us, I had some blurry ideas in my head about clinical trials, like researchers trying to find a cure for a serious condition, spiced with the wild imagination encouraged by the movie industry, where genetic engineering, bio robotics and contagious diseases overwhelm you with alternative live forms and secret experiments.
So, the first step was kind of figuring out what do I deal with, and I started to dig deep into this incredibly documented industry on my own.
Starting with the industry: clinical research is a branch of healthcare science, focusing on determining the safety and effectiveness of medications, devices and diagnostic products. The aim of a clinical research is to collect evidence to establish a treatment and if all goes according to the plan, to get the marketing approval1. And how can they verify their hypotheses? Yes, by studying humans. (Sounds creepy and fascinating at the same time.)
The two main types of trials: interventional and observational studies
Interventional studies are also called clinical trials. It requires participants to take specific interventions as defined in the research plan. Interventions might be a drug, a device, a procedure or any change in the participants’ behavior. Often, trials experiment with new treatments where the effect is not yet known. A new product can be compared with placebo (with no active compound), with other already existing treatments as well as with a control group where no active intervention is applied.
So, in general, trials aim to determine what is the safety and efficacy of an intervention on the human body.
Observational studies are also called epidemiological studies, are those studies where researchers don’t intervene, but rather observe the natural relationship of factors and outcomes. An example could be a study, comparing the prevalence of obesity across different geographic areas where geography is the factor and obesity is the outcome2.
Both interventional and observational study designs have their strengths and weaknesses, which can affect the credibility of the outcome. If you’d like to read more, I recommend the publication of Matthew S. Thiese, who collected several approaches and outlines the pros and cons of each study design.
But the drug development process does not start with the clinical trials. Companies conducting them, have already been through several steps to reach this point.
The everlasting process of drug development
Launching a new product on the pharmaceutical industry takes several years. Researchers and other actors of a clinical trial must agree and follow strict rules outlined by the U.S. Food and Drug Administration (FDA) in the US, or the European Medicines Agency (EMA) in the EU. The rules are set to enforce a standardized drug development process as well as to secure the safety of all involved.
Now let’s see, what stairs need to be climbed before you’ll find a drug on the shelf3, 4:
1. Nonclinical phase
In the nonclinical or pre-clinical phase researchers work on identifying the therapies with the highest probability to be successful. In this phase, they assess the safety of the treatment and establish a foundation for further research5.
The studies in this phase can be performed:
- In silico: via computer simulation
- In vitro: “within the glass”, e.g. experimenting in laboratory environment, using tissues and cells from the human body
- In vivo: “within the living”, using a living organism, mostly in animals
The pre-clinical phase already must align with medical product development regulations and provide detailed information on dosing and toxicity levels which are safe to test on the human body. Typically, to determine the safety, the toxicity should be tested in at least two animal species before being able to move to human testing6. Animal testing is a disputable topic on its own and in the recent years the number of animal testing decreased for both ethical and cost reasons. If you are interested in both sides of the coin though, I recommend reading this article from ProCon.org7.
2. Clinical research
If the research so far complied with regulations and looks promising for further investigation, it can move to the next step: the clinical trial. So far, the team has a lot of information from the pre-clinical phase, but starting the first-in-human trial? That requires a detailed preparation and documentation, almost as specific as the colonization plan of the Moon. Ok, not in that much detail, but I’ll talk about it in Part II: the guidebook of clinical trials.
Now, let’s just focus on the phases of a clinical trial defined by the FDA on their website – yes, more phases are coming within this phase:
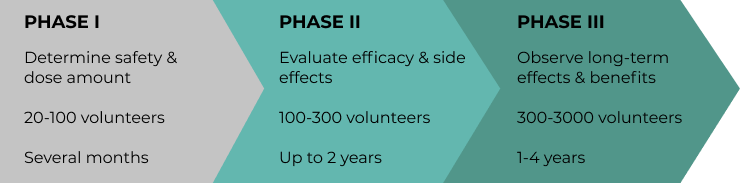
- Phase I: the first-in-human research of the treatment. It takes several months, with a small group (20-100 people). The goal is to evaluate how the human body responds on the intervention. Also, they determine the optimal dose amount and identify side effects within this phase.
- Phase II: this step can last up to 2 years with even several hundred participants with the disease or condition the treatment is developed for. Usually, the information gathered in this phase provides a deeper understanding about the effect and side effects, which will help in designing a research on an even bigger volume: Phase III.
- Phase III: according to the FDA, only 33% of Phase II drugs can reach to Phase III. Studies can last from 1 to 4 years, with 300-3000 participants. At this point, researchers gain insight how effective the treatment is indeed in the analyzed population. Running the study for several years also allows to observe the long-term effects.
3. Regulatory review
After several years of groundwork, if researchers find the treatment to be effective against the disease and safe to the participants, they can file an application for new marketing authorization. The respective regulatory authority will review the request according to the country laws. You can read more about the authorization process in the EU here and in the US here.
4. Post-Marketing
A product reaches the post-marketing stage after the regulatory approval. It’s also called as Phase IV, with the purpose to continue monitoring the safety and to look for rare or long-term side effects which may haven’t occurred in earlier phases. This effort lasts for 2 years minimum, but usually as long as the products stay on the market. Any problems revealed in this phase can result in revoking the product or restricting use. The acne drug Accutane has a controversial story, which medicine Roche stopped manufacturing in 2009. As Reuters cites, it was an economical decision, as generic alternatives gained a bigger share of the market, and not done for safety or efficacy reasons. However, until 2014, more than 7000 lawsuits were filed against Roche, claiming that the drug caused severe side-effects such as birth defects, miscarriage, psychiatric disorders, Crohn’s disease and other stomach issues which people were not warned about. Finally, in 2018 Roche won the litigations and majority of the cases got dismissed, when “the New Jersey Supreme Court ruled that an FDA-approved label is adequate to warn of pharmaceutical side effects”8,9,10.
Huh, so drug development is an awfully long and serious process! Or do you prefer numbers? On average it takes 10 years to bring a drug from the lab tube to the market, and the cost is estimated to be $2.6 billion while the probability of success is only 12%11.
Still, it’s not just the discovery and the fund which make that 12% successful, but all the people who are involved in the process.
The actors involved in clinical trials
So far, I tried to generalize the roles and talked mostly about the participants and researchers as the main driving forces of a trial.
Now, I’ll go through some of the groups in more detail, as many different people are involved during this long journey. And it’s always good to know, who you should ask from the team, when issues occur.
Trial participants
Let’s start with the trial participants, who are referred as “subjects” (sometimes as “patients”). They are the people applied to participate in the study, so they’ll undergo the screening procedure or already receive medication. The participants usually live with the disease or condition a treatment aimed to improve. However, in Phase I studies – the first-in-human stage – in many cases healthy people are involved. In order to enroll, subjects should sign the Informed Consent Form (ICF) where they acknowledge the risks of participation. If you’d raise some ethical concerns at this point, come back later to read the article, where I’ll collect the safety aspects of a clinical trial.
The sponsor
A person, organization, company, institution, voluntary group or government agency that provides funds (money) or other resources for a clinical study.
Moving forward, people in the following roles are core members of the study team, who are involved in the daily activities of the study: the investigator, study coordinator and research nurse12.
The investigator
The investigator is responsible to conduct the study according to the plan on the different locations (also called trial sites, which could be hospitals and other medical institutions). Investigators can be involved in many levels: they can participate in interactions with the patients, conduct data analysis, evaluate the results, serve as biostatisticians and many other activities.
If several investigators are working jointly at the site, their lead is called the principal investigator (PI), who is usually a medical doctor overseeing the complete procedure. The PI is responsible for monitoring the safety of participants and assuring data quality.
Study coordinator
Also called as clinical research coordinator or associate (CRC/CRA). They are heavily involved at the beginning of the process, when participants are evaluated to be fitting to the study criteria: they perform the screening of participants and checking eligibility. During the study, they are collecting and entering the data from visits and other results.
Research nurse
Research nurses hold an active registered nurse (RN) license. Their responsibility is similar to the coordinator but extended with practitioner activities only an RN can perform, like registering the treatment or performing health checks and exams.
Steering Group
Members of the steering group supervise that the study is conducted in an ethical manner and is compliant with the relevant regulations.
Finally, let’s have a section dedicated to the team behind the data.
Data Safety Monitoring Board (DSMB) or Data Monitoring Committee (DMC)
The DSMB is an independent committee, which may be needed to monitor the participants’ safety and efficacy data periodically as well as to provide recommendations for modification.
Clinical data management team
The clinical data management (CDM) team handles the complete life cycle of the data; thus, they are involved from the very first steps of designing a study. Among others, their duties cover the design of electronical forms for collecting the data, the design of database, the validation of data and more13. You can read more about the CDM in Part III: the life cycle of clinical data.
Statistical Programmer
During my work, I mostly collaborated with the statistical programmer team. A statistical programmer plays a key role in code development for analysis and reporting related to a clinical trial. They may serve as a bridge between the sponsor and the study team.
Ok, there you have it! With this short reading I hope you have at least 3 pieces of the puzzle in place now: what is drug development, where clinical trials fit and who plays a key role in the process. Bear with me to the next article, where you’ll learn more about how researchers plan and design the studies!
Resources:
- Learn about clinical studies, clinicaltrials.gov
- Thiese, Matthew S.: Observational and interventional study design types; an overview; Biochem Med (Zagreb). 2014 Jun; 24(2): 199–210.
- The drug development process, fda.gov
- Bere, Nathalie: How are medicines evaluated at the EMA presentation
- Non-clinical development: Basic principles, eupati.eu
- Three major items to consider when moving from preclinical to clinical development, inamed-cro.com
- Should Animals Be Used for Scientific or Commercial Testing?, procon.org
- Accutane side-effects, drugwatch.com
- Accutane lawsuit, drugwatch.com
- Accutane Lawsuits: What’s Happening Now?, enjuris.com
- Biopharmaceutical Research & Development: The Process Behind New Medicines, phrma.org
- Roles in Clinical Research: The Core Study Team, forteresearch.com
- Krishnankutty, Binny, Bellary, Shantala , Kumar, Naveen B.R. and Moodahadu, Latha S.: Data management in clinical research: An overview; Indian J Pharmacol. 2012 Mar-Apr; 44(2): 168–172.

